Inflammation in the body is a good thing … until it’s not. When you suffer an injury or an infection, your body’s immune system quickly dispatches healing cells straight to the source. If you sprain your ankle, for instance, you will almost instantly see and feel the symptoms of acute inflammation, which can be remembered with the acronym PRISH: pain, redness, immobility, swelling, and heat.
This type of inflammation is an essential part of a healthy immune system; it signals that the body is attempting to heal itself, and any pain and immobility you experience are a warning to you to stay off your ankle and employ RICE (rest, ice, compression, and elevation) techniques to ease your discomfort. When the healing process is complete, the inflammatory response normally shuts itself off.
Chronic inflammation, however, is a different story. Because you can’t see or actually feel this type of inflammation, it’s often referred to as the body’s “silent fire”—which makes perfect sense, because the word “inflammation” derives from the Latin word for “to set on fire.” Chronic inflammation occurs when the body’s immune system doesn’t shut off for some reason and begins to burn out of control, like a fire that can’t be extinguished easily. It just keeps producing immune cells, leaving your body in a constant state of alert.
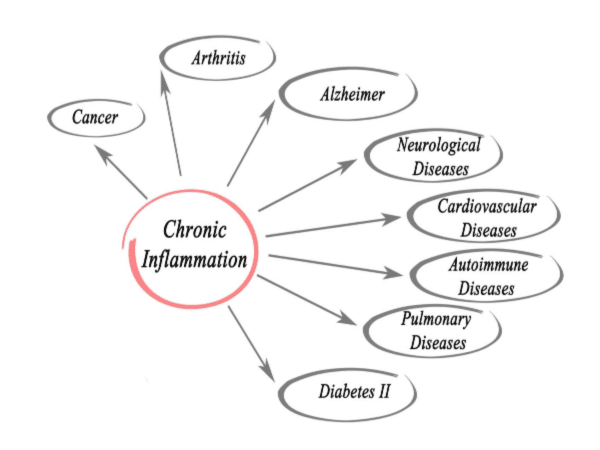
When the immune cells can’t find an injury or illness to repair, they eventually attack healthy cells, damaging your tissues and organs. This sort of damage has been linked to a number of diseases and disorders, including asthma, ulcers, rheumatoid arthritis, heart disease, ulcerative colitis, allergies, some types of cancer and even Alzheimer’s.
“Unfortunately, you can’t see low-grade, chronic inflammation until the damage is already done,” says Desiree Nielsen, a registered dietitian in Vancouver, British Columbia, who focuses on complex chronic digestive and inflammatory disease. The biggest challenge is that it’s largely silent for many of us unless you know what to look for. Chronic inflammation itself can be silent, but of course, the overt diseases aren’t. You may know when you have eczema or diabetes, but you might not realize that it has something to do with inflammation.”
Amy Shah, MD, founder of the website Amy MD Wellness, an online program offering dietary counseling, education, and support for lowering inflammation, compares the body’s inflammatory response to the antivirus software on our computers.
“We know it’s there, doing its job to keep us healthy, but we don’t really notice it until there’s a problem,” Shah says. “Then when there’s a problem, like if we stop exercising, don’t get enough sleep, stress too much, or consume too many processed foods and sugars, our immune system reacts by generating necessary inflammation, just like when your computer software detects an attack.”
THE INFLAMMATION MYSTERY
Although a Roman physician named Celsus first identified the signs (and purpose) of acute inflammation around 30 A.D., research on chronic inflammation didn’t see much progress until the second half of the 20th century, about 2,000 years later, according to the National Institutes of Health (NIH). But physicians, scientists and researchers caution that, despite the current high profile of the issue, there are still a number of unknowns.
“Chronic inflammation is still a mystery,” says Michelle Petri, MD, a rheumatologist and a director of the Johns Hopkins Lupus Center. “The actual triggers and how the inflammation occurs are still not well understood. It’s a combination of genetic, environmental and hormonal factors. In any one patient, we can never give an exact answer about how it all started.”
So, while it’s widely accepted that chronic inflammation can either cause or advance many diseases and disorders, the main question that needs to be answered is how it does that, although there are a number of theories from recent studies.
On the subject of how chronic inflammation can cause digestive issues, a study published in the World Journal of Gastroenterology concluded that “inflammation, regardless of its location or extent, sends many local and systemic signals, which in turn may cause changes in the intestine.” Chronic heart failure, the study reported, is also “associated with increased levels of inflammatory markers.”
And, in a 2017 interview with the American Association for Cancer Research, addressing the correlation between chronic inflammation and cancer, molecular biologist Michael Karin said, “When inflammation goes on for a long time, it can stimulate the growth of cancer cells. This chronic inflammation also inhibits people’s immunity, suppressing the ability of the immune system to recognize cancer as foreign and reject it.”
EXTINGUISHING THE FIRE
Although it’s somewhat difficult to detect the “silent fire” of chronic inflammation, the body offers a number of clues if you’re paying attention.
“Excess inflammation in the body can cause weight gain, especially in the belly; low energy; a mental fog; and an overall ‘blah’ feeling,” Shah says. It can also lead to fatigue, digestive issues, depression, sleep issues, and random aches and pains.
If you’ve been feeling “blah” and there doesn’t seem to be an explanation, Nielsen and Shah advise that the first course of action is to schedule a thorough checkup with your primary care doctor.
“When I’m working with patients, the first step is to determine whether their bodies are inflamed,” Shah says. “I assess things like whether they’re experiencing fatigue, insomnia or bloating, and if they have conditions like allergies, asthma or eczema that are getting worse. Results from certain blood tests can also indicate inflammation.”
Nielsen specifically recommends asking for a blood test to check for C-reactive protein or CRP for short. “It’s a measure of chronic inflammatory response,” she says. “If your levels of CRP register at all, you’ve got some inflammation to fight.” (There are a number of other tests that your doctor might order as well, but no one test gives a complete picture.)
After chronic inflammation is diagnosed, Nielsen and Shah both help people adopt an anti-inflammatory lifestyle, a major component of which is diet.
An anti-inflammatory diet, Nielsen says, is largely a plant-based one. “The digestive tract is a primary target for anti-inflammatory efforts, as 80 percent of the immune system is located within the gut, and gut microbes can drive inflammation.”
There are four main goals of an anti-inflammatory diet, explains Nielsen. “You want to keep blood sugars balanced, eat the right types of fats, consume anti-inflammatory phytochemicals and promote healthy gut flora.”
After Lora Fisher of Santa Barbara, California, was diagnosed with chronic inflammation, she cut out flour, high-salt foods and added sugar, and started eating more whole foods. “I felt better within a few weeks,” she says, “and I learned which foods will trigger the pain and swelling. I now know to avoid those foods, and I know I’ll be sorry if I do consume them.”
While carefully monitoring what you eat is crucial for reducing inflammation, Shah and Nielsen agree, there are other steps to take, including adopting a relaxing, presleep ritual; learning how to breathe deeply during periods of stress; exercising more; reducing caffeine and alcohol intake.
“The good news,” Shah adds, “is that making a few small changes, for just a few minutes each day, can help to dramatically lower inflammation levels in the body.
UN-JUNK YOUR DIET
Anti-inflammatory eating tips from Desiree Nielsen, RD. Check off the healthy eating tips you’re already doing, and to reveal where you can focus your efforts on to help your body ward off chronic inflammation.
- Load at least half your plate with vegetables and fruits at every meal.
- Get anti-inflammatory phytochemicals from flavonoids in raw cocoa, tea and berries; carotenoids in yellow and orange vegetables, such as carrots; and anthocyanins in red fruits and vegetables, such as strawberries, raspberries, red peppers, and red apples.
- Layer in plant proteins, like organic tofu, legumes and some eggs (and some non-plant proteins like poultry or fish, if you consume them).
- Dump processed grains in favor of whole, intact grains, such as steel-cut oats, millet, and barley.
- Enjoy healthful fats, such as olives and avocados and their oils.
- Snack on raw nuts and seeds.
- Eat fermented foods daily, like unpasteurized sauerkraut and kombucha.
- For supercharged nutrition, consume berries, leafy greens, matcha, mushrooms and brassicas (such as cauliflower) daily.
- Eliminate refined flours.
- Lower your overall sugar intake (even from natural sugars like date pastes and maple syrup).
- Avoid concentrated sources of omega-6 fats from oils like soy, canola or corn.
- Supplement with vitamin D, probiotics and omega-3 fatty acids.
Author Credit: Lisa Truesdale
Lisa Truesdale is a health freelancer writer, editor, proofreader and blogger.
[contentblock id=9 img=gcb.png]




What a fabulous post about ways to extinguish chronic inflammation. In fact I included a link to it on my blog (and provided source) and pinned this post. I’m visiting from Pretty Pintastic Pin Party #266 where I shared 9 Practices to Help Us See We Are Enough and Bloom into Health Eat Color Rich Produce. Thanks for hosting!
Glad you found the post informative. Thanks for stopping by and sharing on your blog.
This has been debilitating in my life since 03. Horrible pain.
I’ve had high CRP levels so I had to change my diet just as you recommended. I eat a lot of fruit and veg now, I don’t do any dairy, and eggs were bothersome for me. I try to stay fairly low-fat and use extra virgin olive, coconut, or avocado oils. I also cut out gluten and don’t eat very many grains. It takes a lifestyle shift but it’s worth it I think.
Just like one size never fits all one diet (nutrition plan) never fits all. It’s about what your body needs. I am glad you found what works for you. Thanks for sharing your experience.